Regulators Approve Lenacapavir for H.I.V. Prevention


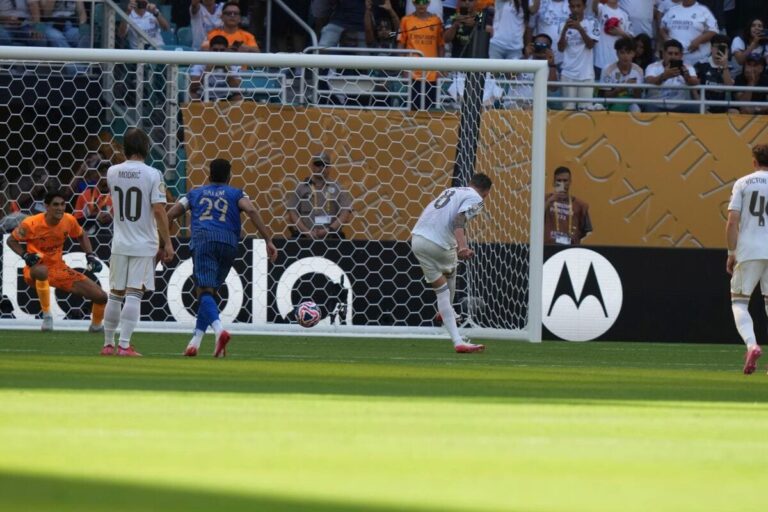
The drug could change the course of the AIDS epidemic. But the Trump administration has gutted the programs that might have paid for it in low-income countries. The Food and Drug Administration on Wednesday approved a twice-yearly injection that provided a near-perfect shield against H.I.V. infection in clinical trials. The approval is among the most anticipated developments in the prevention of H.I.V. But it arrives during deep cuts to global health programs that were expected to purchase and distribute the drug in low-income countries. To what extent the drug, called lenacapavir, can now be rolled out is uncertain. “We’re on the precipice of now being able to deliver the greatest prevention option we’ve had in 44 years of this epidemic,” said Mitchell Warren, executive director of the international H.I.V. prevention organization AVAC. “And it’s as if that opportunity is being snatched out of our hands by the policies of the last five months,” he said. With much less money available, governments abroad may instead choose to prioritize treatment of the infected. “We were so excited about the possibilities,” said Dr. Linda-Gail Bekker, who led a clinical trial of the drug. “I don’t think any of us envisaged this year going quite the way it has.” Lenacapavir, made by Gilead Sciences and to be marketed as Yeztugo, is the second long-acting option for H.I.V. prevention. An alternative, cabotegravir (brand name Apretude), is a shot given every two months and is made by ViiV Healthcare, GSK’s H.I.V. company. Apretude is given to roughly 21,000 Americans, while daily pills to prevent H.I.V. are taken by nearly 500,000. Many public health experts believe that the convenience of a twice-yearly injection has the potential to transform the epidemic. In clinical trials, lenacapavir surpassed expectations: Participants given just two shots each year were almost completely protected. In the United States, more than 39,000 people contracted H.I.V. in 2023. Every newly infected person incurs about $1.1 million in medical care over his or her lifetime, Daniel O’Day, Gilead’s chairman and chief executive officer, said in an interview. Prevention is “the most cost-effective way of bending the arc of this epidemic,” he added. Lenacapavir is already sold as a treatment for H.I.V. infections that are resistant to other medications, at roughly $42,000 per patient per year. (Few individuals pay the full cost.) Lenacapavir taken to prevent H.I.V. infection, a regimen called pre-exposure prophylaxis, or PrEP, will be sold at a list price of $28,218, according to Gilead. While the price for generic oral pills now is as little as $1 per dose, the other long-term option, Apretude, costs roughly $24,000 per year. Gilead said most people would not have to pay for the drug, either because of insurance coverage, or through patient assistance programs. But advocacy organizations worry that insurance companies may raise barriers to widespread availability. “In the U.S., we’re anticipating that history will repeat itself with lenacapavir, with widespread access being thwarted by many of the same pricing and coverage nightmares we saw with the launch of daily oral PrEP and Apretude,” said Jeremiah Johnson, executive director of the advocacy organization PrEP4All. Proposed cuts to Medicaid in the proposed budget now before the Senate also would restrict access for many Americans most at risk of H.I.V. infection, he added. States that expanded Medicaid have 33 percent more people on PrEP than other states. The need for prevention is even more acute elsewhere in the world. Globally, about 1.3 million people became infected with H.I.V. in 2023. Last year, Gilead said it would allow six companies worldwide to make and sell lenacapavir at affordable prices to 120 low-income nations. Until those companies are able to meet demand, which may take two to three years, Gilead will provide the drug as a preventative at “no-profit costs” to two million people in those countries, Mr. O’Day said. But the agreement does not extend to the middle-income countries, including Brazil, which together account for nearly one in four new H.I.V. infections. Gilead has filed for regulatory approval in Brazil, and is negotiating with other middle-income countries to settle on prices, according to the company. The drug will also be available to a few thousand people in Brazil, South Africa and the United States who enroll in research studies. Still, “this is a profound barrier to access and means millions of people will be consigned to second-class PrEP that science has shown us does not work for them,” said Asia Russell, executive director of the advocacy group Health Gap, referring to daily oral pills. The policy bill under review in the Senate would shrink funding for the President’s Emergency Program for AIDS Relief, or PEPFAR, and the Global Fund to Fight AIDS, Tuberculosis and Malaria, which probably would have been the largest buyers of lenacapavir. In January, the Trump administration halted disbursement of funds from PEPFAR, which supplied most of the treatment for H.I.V. in low-income countries worldwide. The State Department later issued waivers to allow treatments to resume, but did not restore funding for H.I.V. prevention. The only exception is to prevent transmission of the virus from a pregnant woman to her child. Other donor organizations, including the Gates Foundation, have not shown an interest in purchasing lenacapavir. “My great concern is that we will miss this moment and not build the market for generics in the next two or three years if we don’t work with Gilead,” Mr. Warren said. Within the United States, too, the Trump administration has hobbled efforts to prevent H.I.V. transmission. It has withheld funds that were due to states and territories for the effort, and the National Institutes of Health has terminated several grants related to research into preventive drugs. “Prevention just feels hugely at risk writ large,” Dr. Bekker said. “If we don’t prevent this epidemic, it will just drag on and on and on.”
What's Your Reaction?
 Like
0
Like
0
 Dislike
0
Dislike
0
 Love
0
Love
0
 Funny
0
Funny
0
 Angry
0
Angry
0
 Sad
0
Sad
0
 Wow
0
Wow
0